Neurological Diagnostic Tests
Neurological Diagnostic Tests
Some common neurological diagnostic tests available to patient by referrals
Angiogram
CT Scan
PET Scan
Magnetic Resonance Imaging (MRI)
Evoked Potentials (EP)
Carotid Ultrasound
Angiogram
 Angiography is a diagnostic imaging technology in which a contrast dye is injected directly into a blood vessel through a thin tube (catheter). The dye is captured on x-ray film as it passes through the vessel, and the resulting picture is called an angiogram. Sometimes a set of pictures can be combined like frames in a movie to capture motion. If there is a problem area, it may appear as a narrowing, bloackage, or spot in the vessel.
Angiography is a diagnostic imaging technology in which a contrast dye is injected directly into a blood vessel through a thin tube (catheter). The dye is captured on x-ray film as it passes through the vessel, and the resulting picture is called an angiogram. Sometimes a set of pictures can be combined like frames in a movie to capture motion. If there is a problem area, it may appear as a narrowing, bloackage, or spot in the vessel.
Most angiograms focus on the brain, heart, lungs, head, neck, arms, legs or the aorta (the main artery carrying blood from the heart). The catheter is most often inserted into the femoral vein or artery, both located in the groin area.
Angiograms reveal problems occurring in blood vessels—particularly those in or surrounding the brain and heart. An angiogram will display how blood moves around an obstruction such as a clot, as well as through a narrowing in a blood vessel wall. It can also show where a weakness in an artery wall could lead to an aneurysm.
Cerebral angiograms are mainly concerned with diagnosing problems in the blood vessels of the brain. Neurologists sometimes rely on this procedure to evaluate an abnormal blood vessel, check for an aneurysm, assess the narrowing of an artery, confirm or check a brain tumor, locate a clot that could cause a stroke, or check arteries before performing surgery. Other neurological conditions that might call for an angiogram include swelling (edema) of the brain, narrowing caused by a spasm (vasospasm), increased intracranial pressure (ICP) or fluid within the brain (hydrocephalus).
Interventional angiograms: In some cases, doctors performing a diagnostic angiogram might use the catheter to actually treat a problem. In addition to delivering contrast dye used in imaging studies, the catheter might be used to:
- Deliver medication to the site of a stroke or tumor
- Reopen a blocked brain artery
- Stop internal bleeding
CT Scan
 A Computed Tomography (CT or CAT) scan is a medical diagnostic procedure that combines nuclear radiation and x-ray technologies to create highly detailed images of the body. Instead of a single flat 2-dimensional picture produced by a stationary x-ray camera, a CT scanner provides a series of cross-sectional images that are “stacked” together on a computer to reveal the depth of an image in striking detail.
A Computed Tomography (CT or CAT) scan is a medical diagnostic procedure that combines nuclear radiation and x-ray technologies to create highly detailed images of the body. Instead of a single flat 2-dimensional picture produced by a stationary x-ray camera, a CT scanner provides a series of cross-sectional images that are “stacked” together on a computer to reveal the depth of an image in striking detail.
The images are obtained by holding the area to be studied perfectly still and rotating an x-ray camera over the area. This results in multiple views taken from different vantage points. These individual images provide a clear 3-dimensional effect that helps doctors diagnose a wide range of conditions.
A CT scan can painlessly look through dense objects such as bones to see organs and structures behind them. And it can look inside dense objects to provide an interior view. In some cases a contrast dye, administered through an IV line or swallowed, enhances the quality of the images. These capabilities make CT scans ideal for fine-tuned diagnostic pictures of whole areas of the body as well as most of the specific organs and other structures.
Recent technological advances have enabled several variations on CT technology. Among them:
- Computed Tomographic Angiography (CTA) for imaging blood vessels.
- High-Resolution Computed Tomography for even sharper images and greater detail.
- Ultrafast Computed Tomography to show motion such as the heart beating. This is also known as Electron Beam Computed Tomography.
- Helical or Spiral Computed Tomography for scans that are more detailed and obtained faster than regular CT.
- Positron Emission / Computed Tomography (PET/CT) for combining both technologies. PET/CT scans reveal anatomic details as well as studies of cell function and metabolism in a single series of images.
CT scans help doctors diagnose problems associated with illness and injury. The images sometimes aid in monitoring the progress of diseases and guiding delicate procedures and surgeries. They can provide a reliable, clear view of organs, structures and whole regions of the body, from head to toe.
In the brain, the organ of greatest interest to neurologists, CT scans help physicians perform a wide range of important tasks. These include
- Rapidly diagnosing a stroke and pinpointing the location of the blood clot or aneurysm that could have caused it.
- Detecting damage to the brain or skull that comes from a head injury.
- Assessing the size, shape and location of a brain tumor.
- Identifying the location of a potentially fatal brain aneurysm.
- Monitoring the advancement of progressive diseases like Multiple Sclerosis (MS), Parkinson’s disease and other neurological disorders.
- Providing clear, detailed images of the brain cavity, which is important when a patient has hydrocephalus.
CT scans also help neurosurgeons plan facial reconstruction and other surgeries as well as procedures like radiation therapy for brain cancer and biopsy of brain tissue.
Of course neurologists and neurosurgeons are not the only medical professionals who rely on CT scans. The same equipment is commonly used to create images throughout the body. Some of the reasons other physicians might request a CT scan include:
- Assessing damage from internal injuries and bleeding.
- Checking the spread of cancer and other progressive diseases.
- Zeroing in on the precise location of a tumor, blood clot or infection. This is particularly useful in biopsies, radiation therapy and some kinds of surgery.
- Examining the chest and abdomen for problems such as embolism, aneurysm, cysts, abscesses, foreign objects, enlarged lymph nodes, infections and others.
- Locating problems in the urinary tract such as blockages, growths and kidney and bladder stones.
- Checking for problems in the abdominal organs, including the liver, pancreas, adrenal glands and spleen.
- Imaging the structures and organs in the pelvic region—ovaries, uterus and fallopian tubes in women, or prostate gland and seminal vesicles in men.
- Examining damage to the extremities, including the arms and legs, hands, wrists, elbows and shoulders, feet, ankles, knees and hips.
PET Scan
 Positron Emission Tomography (PET) is a nuclear imaging technology that uses radioactive material to show biological processes as they occur inside the body. The technology produces images that are used by physicians to diagnose medical problems and establish what might be causing them. In this way, PET scans help doctors determine what treatment is best for a patient.
Positron Emission Tomography (PET) is a nuclear imaging technology that uses radioactive material to show biological processes as they occur inside the body. The technology produces images that are used by physicians to diagnose medical problems and establish what might be causing them. In this way, PET scans help doctors determine what treatment is best for a patient.
PET scans are used primarily to help diagnose problems in the nervous system, brain or heart, as well as many kinds of cancer throughout the body.
The radioactive material (called a tracer, radionuclide or radiopharmaceutical) is a chemical that’s inhaled or injected into the body through an IV and emits atomic particles called positrons. These positrons accumulate in the area being studied—an organ or tissue, typically—and are detected by a camera that records data for analysis by a computer. The computer converts all this information into an image.
What makes PET scans different from Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and other imaging technology is that PET scans can detect metabolism (the process that converts nutrients into energy) occurring in an organ or tissue. This means PET scans can sometimes show a disease process that’s occurring before other imaging technologies can detect the damage (changes in the structure of the organ or tissue) done by the disease process. In fact, PET scan images are sometimes combined with CT or MRI images to produce more detailed pictures.
Doctors might order a PET scan when they need more than a static image of damage already done to the patient’s body. PET technology lets doctors look at the metabolic process (i.e. how the cells convert oxygen and other nutrients in the blood into energy) occurring within the tissue being studied. In some situations, this provides an early glimpse of possible disease processes at work even before the damage from those processes is apparent.
Neurological conditions that might need a PET scan:
- Alzheimer’s disease
- Amyotrophic Lateral Sclerosis (ALS)
- dementias
- Epilepsy and seizures
- Head trauma
- Huntington’s disease
- Multiple Sclerosis (MS)
- Parkinson’s disease
- Stroke
- Transient Ischemic Attack (TIA)
Cancer: A PET scan can sometimes detect cancer before other kinds of imaging can. It can indicate how advanced a cancer is, show if it has spread, and help a physician determine if a tumor is operable—and exactly where to operate. Cancers that might need a PET scan include:
- Brain Cancer
- Breast Cancer
- Colon Cancer
- Lung Cancer
- Lymphona
- Prostate Cancer
Heart disease: Doctors rely on PET scans to help diagnose and pinpoint treatment options for heart attack, atherosclerosis and other conditions.
Magnetic Resonance Imaging (MRI)
 MRI is a diagnostic imaging technology that gives physicians a detailed picture of part of the body. It produces digital images that can be stored on a computer and manipulated for further study. The images help doctors diagnose problems with a high degree of accuracy.
MRI is a diagnostic imaging technology that gives physicians a detailed picture of part of the body. It produces digital images that can be stored on a computer and manipulated for further study. The images help doctors diagnose problems with a high degree of accuracy.
MRI has its own set of advantages and limitations in specific situations. It is not used to treat medical conditions, but is often instrumental in helping doctors determine what treatment(s) will work best.
Variations: With MRI technology as a starting point, medical science has developed similar procedures that help physicians diagnose even more conditions with the same pinpoint accuracy. Variations include:
- Magnetic Resonance Angiography (MRA): Used for non-invasive evaluation of blood flow through arteries. MRA can also detect aneurysms and other blood vessel abnormalities within the brain, spinal cord, or other parts of the body.
- Magnetic Resonance Spectroscopy (MRS): Used for assessing chemical abnormalities in body tissues like the brain. MRS can examine disorders such as HIV infection of the brain, stroke, head injury, coma, Alzheimer’s disease, tumors, and Multiple Sclerosis (MS).
- Functional Magnetic Resonance Imaging (fMRI): Used for determining the specific location in the brain where a certain function, such as speech or memory, occurs. These locations vary slightly for each patient. Knowing where these functional areas are located helps physicians plan surgery or other treatments for a particular disorder.
Physicians use MRI to help diagnose a wide range of conditions, diseases, abnormalities and injuries. Unlike other kinds of imaging, MRI can “see” through bones, like the skull and vertebrae, to pinpoint an area of an organ or soft tissue. MRI doesn’t expose the patient or technician to radiation.
Some common medical situations where neurologists might need an MRI include Multiple Sclerosis (MS) and other degenerative diseases, as well as stroke, tumors, aneurysms, abscesses, congenital abnormalities, hydrocephalus and many others. MRI technology is also helpful in diagnosing:
- Hypoxic encephalopathy (dysfunction of the brain due to a lack of oxygen)
- Encephalomyelitis (inflammation or infection of the brain and/or spinal cord)
- Herniated or degenerated discs of the spinal cord
- Malformations of veins and/or arteries of the brain or spinal cord
- Hemorrhage, or bleeding into the brain or spinal cord
- Subdural hematoma (bleeding just under the brain’s protective covering)
If an MRI has been recommended for you, or you’re scheduled to receive one, you probably wonder what it will be like. The procedure is painless. If you’re claustrophobic, you can request an Open MRI. A mild sedative is available if you need it.
Evoked Potentials (EP)
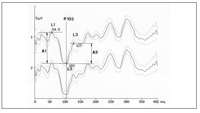 Evoked Potentials (EP) tests are used to check the condition of the nerve pathways. They measure the brain’s electrical response to the signals sent by the nerves. EP tests help diagnose nervous system abnormalities, hearing loss, and assess neurological functions.
Evoked Potentials (EP) tests are used to check the condition of the nerve pathways. They measure the brain’s electrical response to the signals sent by the nerves. EP tests help diagnose nervous system abnormalities, hearing loss, and assess neurological functions.
Major Types of Evoked Potentials (EP) Tests
- Brainstem Auditory Evoked Potential – Checks the pathway from the ear to the brain. The BAEP test may help uncover the cause of hearing and balance problems, and other symptoms.
- Visual Evoked Potential – Checks the pathway from the eyes to the brain. May help find the cause of certain vision problems and other conditions.
- Somatosensory Evoked Potential – Checks the pathway from the nerves in the limbs to the brain. It is a way to study the function of the nerves, the spinal cord and brain.
Preparation:
- Wash your hair the night before the test. Do not use any oils or lotions.
- Eat a normal meal at your usual mealtime before the test.
- Avoid caffeine.
- Bring glasses or contact lenses for the Visual Evoked Potential test. Procedure: • Positioned on a reclining chair or bed and asked to relax, remain still. • Electrodes placed on your scalp, along the vertex and on each earlobe. • A mild stimulus is applied to the eyes, ears or limbs. • Clicking noises or tone bursts heard through earphones. • The electrodes pick up the brain’s response and record it on a graph. How It Feels
Procedure:
- Positioned on a reclining chair or bed and asked to relax, remain still.
- Electrodes placed on your scalp, along the vertex and on each earlobe.
- A mild stimulus is applied to the eyes, ears or limbs.
- Clicking noises or tone bursts heard through earphones.
- The electrodes pick up the brain’s response and record it on a graph.
How It Feels:
- Very little discomfort is experienced.
The test is usually performed within an hour, and is painless and safe.
Carotid Ultrasound
 Ultrasound uses sound waves instead of radiation to generate snapshots or moving pictures of structures inside the body.
Ultrasound uses sound waves instead of radiation to generate snapshots or moving pictures of structures inside the body.
Carotid duplex ultrasonography (CUS) is a useful diagnostic tool for assessing cervical carotid artery disease.
A Carotid ultrasound shows the amount of blood flow in the carotid arteries, the major blood vessels to the brain located on either side of your neck. With this imaging technique, your doctor can see if there is any narrowing of your carotid arteries because of cholesterol deposits or some other problem. This test is often used to evaluate people who have had a stroke or who might be at high risk for one because of reduced blood flow in the carotid arteries.
Preparation:
There is no preparation required for this test.
Procedure:
A technician places the sensor against your skin using a clear gel for application. As the technician moves the sensor back and forth on your neck, different views of the carotid artery appear on the screen. As the equipment measures the blood flow through the artery, you hear a noise that sounds like your heartbeat. The other side of your neck is checked in the same way. This test usually takes 15–30 minutes.
How It Feels:
This procedure is painless.