- Electromyogram (EMG) (NCS)

- The presence, size, and shape of the wave form produced on the oscilloscope (the action potential) provide information about the ability of the muscle to respond to nervous stimulation.
- Each muscle fiber that contracts will produce an action potential and the size of the muscle fiber affects the rate (how frequently an action potential occurs) and size (amplitude) of the action potential(s).
An EMG may be used to evaluate a variety of problems, including the following:
- Nerve damage from compression by a disk in the neck or the back
- Nerve compression from carpal tunnel syndrome
- Neuromuscular diseases such as amyotrophic lateral sclerosis (ALS), poliomyelitis, myasthenia gravis and muscular dystrophy
- Peripheral neuropathy caused by such conditions as diabetes, pernicious anemia and heavy metal toxicity
In many instances, an EMG can provide critical diagnostic information that can not be obtained in any other way.
Although there is some discomfort associated with the procedure, an EMG is usually done on an outpatient basis.
Preparation
No special preparation is usually necessary.
Procedure
- The electrical activity detected by this electrode is displayed on an oscilloscope.
- You may be asked to contract the muscle.
- To perform intramuscular EMG, a needle electrode is inserted through the skin into the muscle tissue. A trained medical professional observes the electrical activity while inserting the electrode.
- Nerve Conduction Study (NCS)
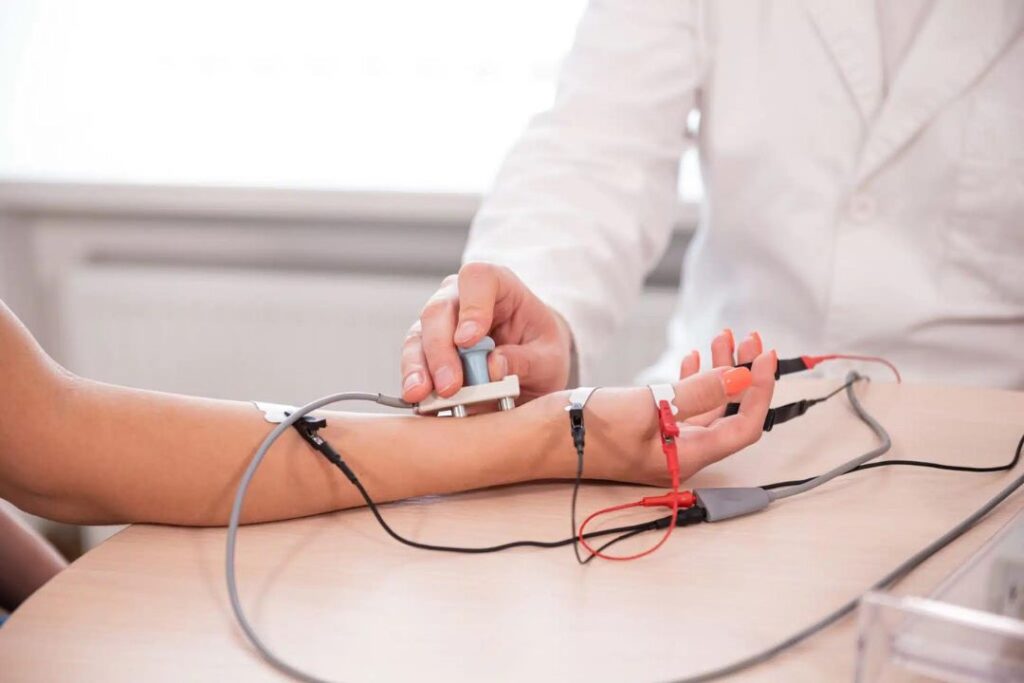
A nerve conduction study (NCS) is a test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body.
Nerve conduction studies are mainly used for the evaluation of paresthesias (numbness, tingling, burning) and/or weakness of the arms and legs. It can be used to diagnose disorders of the peripheral nerves and muscles.An EMG is done by inserting electrodes in fine needles into the muscles being tested, and by placing electrodes on the skin over peripheral nerves.
How It Feels
The test is not invasive, but can be a little painful due to the electrical shocks. However, the shocks are associated with such a low amount of electrical current that they are not dangerous to anyone.
There should be no residual pain once the test is finished.
Preparation:
Normal body temperature must be maintained (low body temperature slows nerve conduction).
Procedure:
The nerve is stimulated, usually with surface electrodes, which are patch-like electrodes (similar to those used for ECG) placed on the skin over the nerve at various locations. One electrode stimulates the nerve with a very mild electrical impulse. The resulting electrical activity is recorded by the other electrodes. The distance between electrodes and the time it takes for electrical impulses to travel between electrodes are used to calculate the nerve conduction velocity. Electromyography is the second part of this test and is often done within one week of the NCS.
How It Feels
The test is not invasive, but can be a little painful due to the electrical shocks. However, the shocks are associated with such a low amount of electrical current that they are not dangerous to anyone.
There should be no residual pain once the test is finished.
Preparation:
Normal body temperature must be maintained (low body temperature slows nerve conduction).
Procedure:
The nerve is stimulated, usually with surface electrodes, which are patch-like electrodes (similar to those used for ECG) placed on the skin over the nerve at various locations. One electrode stimulates the nerve with a very mild electrical impulse. The resulting electrical activity is recorded by the other electrodes. The distance between electrodes and the time it takes for electrical impulses to travel between electrodes are used to calculate the nerve conduction velocity. Electromyography is the second part of this test and is often done within one week of the NCS.
- Nerve Conduction Study (NCS)
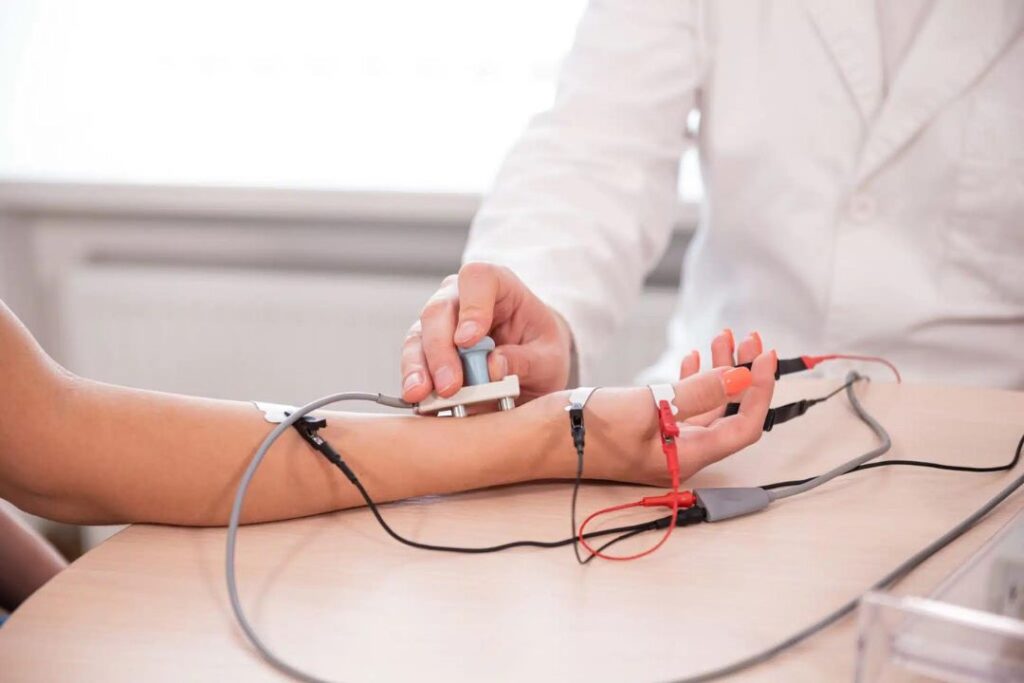
A nerve conduction study (NCS) is a test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body.
Nerve conduction studies are mainly used for the evaluation of paresthesias (numbness, tingling, burning) and/or weakness of the arms and legs. It can be used to diagnose disorders of the peripheral nerves and muscles.An EMG is done by inserting electrodes in fine needles into the muscles being tested, and by placing electrodes on the skin over peripheral nerves.
- Electroencephalogram (EEG)
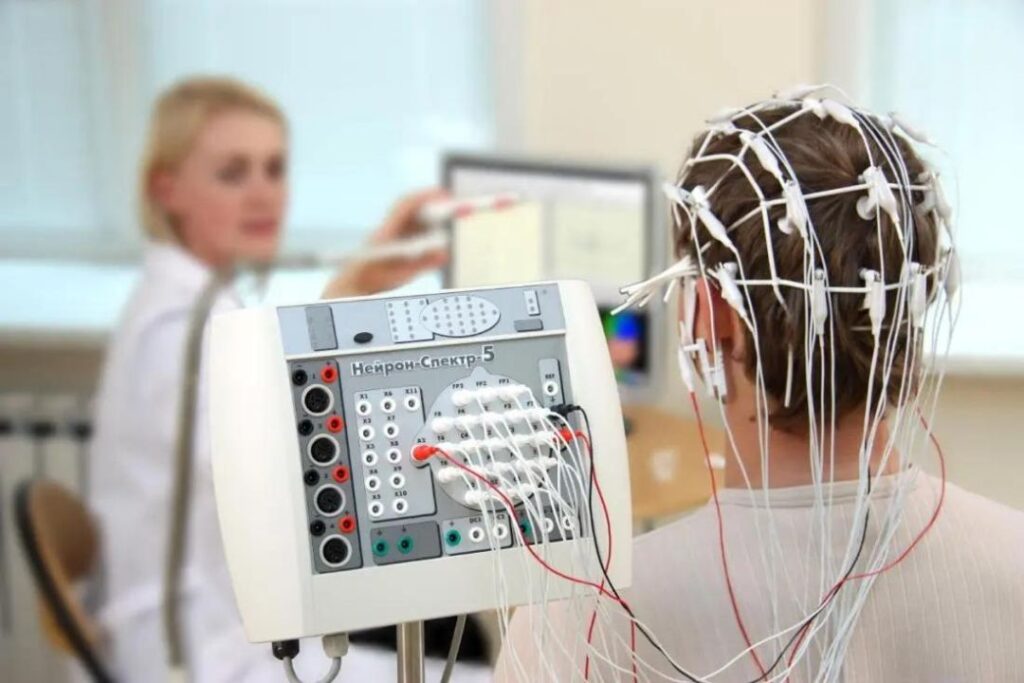
Electroencephalography (EEG) is the measurement of electrical activity produced by the brain as recorded from electrodes placed on the scalp.
An EEG is used to help diagnose the presence and type of seizure disorders, confusion, head injuries, brain tumors, infections, degenerative diseases, and metabolic disturbances that affect the brain. It is also used to evaluate sleep disorders and to investigate periods of unconsciousness. Nerve conduction studies are mainly used for the evaluation of paresthesias (numbness, tingling, burning) and/or weakness of the arms and legs. It can be used to diagnose disorders of the peripheral nerves and muscles. An EMG is done by inserting electrodes in fine needles into the muscles being tested, and by placing electrodes on the skin over peripheral nerves.
How It Feels
This procedure is painless.
Preparation:
- Please wash your hair the night before the test. No oils, sprays, or lotion should be used on your hair.
- Please avoid all foods/drinks containing caffeine for 8 hours before the test.
- It may be necessary to sleep during the test, so you may be asked to reduce your sleep time the night before.
Procedure:
- This procedure is performed by an EEG technician and typically lasts 20-40 minutes.
- You may be positioned on your back, on a table, or in a reclining chair.
- The technician will apply between 16 and 25 flat metal discs (electrodes) in different positions on your scalp.
- The discs are held in place with a sticky paste. The electrodes are connected by wires to an amplifier and the recording machine which converts the electrical signals into a series of wavy lines which are drawn onto a moving piece of graph paper.
- Cerebral spinal fluid (CSF)

Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. Cerebrospinal fluid acts as a cushion, protecting the brain and spine from injury. The fluid is normally clear. The test is also used to measure pressure in the spinal fluid.
How the Test is Performed
There are different ways to get a sample of CSF. Lumbar puncture, commonly called a spinal tap, is the most common method. The test is usually done like this:
- The patient lies on his or her side, with knees pulled up toward the chest, and chin tucked downward. Sometimes the test is done with the person sitting up, but bent forward.
- After the back is cleaned, the health care provider will inject a local numbing medicine (anesthetic) into the lower spine.
- A spinal needle is inserted, usually into the lower back area.
- Once the needle is properly positioned, CSF pressure is measured and a sample is collected.
- The needle is removed, the area is cleaned, and a bandage is placed over the needle site. The person is often asked to lie down for a short time after the test.
Why the Test is Performed
This test is done to measure pressures within the cerebrospinal fluid and to collect a sample of the fluid for further testing. CSF analysis can be used to diagnose certain neurologic disorders, particularly infections (such as meningitis) and brain or spinal cord damage.
Occasionally, special x-rays are used to help guide the needle into the proper position. This is called fluoroscopy.
Lumbar puncture with fluid collection may also be part of other procedures, particularly a myelogram (x-ray or CT scan after dye has been inserted into the CSF).
Alternative methods of CSF collection are rarely used, but may be necessary if the person has a back deformity or an infection.
Cisternal puncture uses a needle placed below the occipital bone (back of the skull). It can be dangerous because it is so close to the brain stem. It is always done with fluoroscopy.
Ventricular puncture is even more rare, but may be recommended in people with possible brain herniation. This test is usually done in the operating room. A hole is drilled in the skull, and a needle is inserted directly into one of brain’s ventricles.
CSF may also be collected from a tube that’s already placed in the fluid, such as a shunt or a venitricular drain. These sorts of tubes are usually placed in the intensive care unit.
How to Prepare for the Test
The patient (or guardian) must give the health care team permission to do the test.
Afterward, you should plan to rest for several hours, even if you feel fine. You won’t be required to lie flat on your back the entire time, but rest is advised to prevent additional leakage of CSF around the site of the puncture.
How the Test Will Feel
The test is usually done with you curled up on your side with knees pulled up and chin to chest. Sometimes, CSF is collected with the person seated and bent forward over a table or chair. Holding the position may be uncomfortable, but it is extremely important to stay in this bent position to avoid moving the needle and possibly injuring the spinal cord. The person doing the test may ask you to straighten out slightly after the needle is in place, in order to accurately measure the CSF pressure, called the “opening pressure.”
The anesthetic will sting or burn when first injected. There will be a hard pressure sensation when the needle is inserted, and there is usually some brief pain when the needle goes through the tissue surrounding the spinal cord. This pain should stop in a few seconds.
Overall, discomfort is minimal to moderate. The entire procedure usually takes about 30 minutes, but it may take longer. The actual pressure measurements and CSF collection only take a few minutes.
Occasionally, special x-rays are used to help guide the needle into the proper position. This is called fluoroscopy.
Lumbar puncture with fluid collection may also be part of other procedures, particularly a myelogram (x-ray or CT scan after dye has been inserted into the CSF).
Alternative methods of CSF collection are rarely used, but may be necessary if the person has a back deformity or an infection.
Cisternal puncture uses a needle placed below the occipital bone (back of the skull). It can be dangerous because it is so close to the brain stem. It is always done with fluoroscopy.
Ventricular puncture is even more rare, but may be recommended in people with possible brain herniation. This test is usually done in the operating room. A hole is drilled in the skull, and a needle is inserted directly into one of brain’s ventricles.
CSF may also be collected from a tube that’s already placed in the fluid, such as a shunt or a venitricular drain. These sorts of tubes are usually placed in the intensive care unit.
How to Prepare for the Test
The patient (or guardian) must give the health care team permission to do the test.
Afterward, you should plan to rest for several hours, even if you feel fine. You won’t be required to lie flat on your back the entire time, but rest is advised to prevent additional leakage of CSF around the site of the puncture.
How the Test Will Feel
The test is usually done with you curled up on your side with knees pulled up and chin to chest. Sometimes, CSF is collected with the person seated and bent forward over a table or chair. Holding the position may be uncomfortable, but it is extremely important to stay in this bent position to avoid moving the needle and possibly injuring the spinal cord. The person doing the test may ask you to straighten out slightly after the needle is in place, in order to accurately measure the CSF pressure, called the “opening pressure.”
The anesthetic will sting or burn when first injected. There will be a hard pressure sensation when the needle is inserted, and there is usually some brief pain when the needle goes through the tissue surrounding the spinal cord. This pain should stop in a few seconds.
Overall, discomfort is minimal to moderate. The entire procedure usually takes about 30 minutes, but it may take longer. The actual pressure measurements and CSF collection only take a few minutes.
- Cerebral spinal fluid (CSF)

Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. Cerebrospinal fluid acts as a cushion, protecting the brain and spine from injury. The fluid is normally clear. The test is also used to measure pressure in the spinal fluid.
How the Test is Performed
There are different ways to get a sample of CSF. Lumbar puncture, commonly called a spinal tap, is the most common method. The test is usually done like this:
- The patient lies on his or her side, with knees pulled up toward the chest, and chin tucked downward. Sometimes the test is done with the person sitting up, but bent forward.
- After the back is cleaned, the health care provider will inject a local numbing medicine (anesthetic) into the lower spine.
- A spinal needle is inserted, usually into the lower back area.
- Once the needle is properly positioned, CSF pressure is measured and a sample is collected.
- The needle is removed, the area is cleaned, and a bandage is placed over the needle site. The person is often asked to lie down for a short time after the test.
Why the Test is Performed
This test is done to measure pressures within the cerebrospinal fluid and to collect a sample of the fluid for further testing. CSF analysis can be used to diagnose certain neurologic disorders, particularly infections (such as meningitis) and brain or spinal cord damage.
